Predictability: The Best Way to Protect Your Value-Based Care Model
The COVID-19 outbreak in the U.S. has exposed many shortcomings in our current healthcare system. One of those shortcomings is how value-based delivery models, such as accountable care organizations (ACOs), are currently structured.
It’s critical for hospitals, health systems and medical practices to know their patient populations. Otherwise, these organizations can’t accurately predict the costs of patient care and how much revenue to expect from payer partners to cover those costs.
Difficulty in predicting value-based payments was the theme of a recent survey of 304 executives at 226 Medicare ACOs conducted by the National Association of ACOs (NAACOS).
“When ACOs made a commitment to assume risk, they didn’t expect they’d be handling the risk of a global pandemic.”
– Clif Gaus, NAACOS president and CEO
The ACOs surveyed all participate in the Medicare Shared Savings Program and the Next Generation ACO Model program. In both programs, ACOs assume the financial risk of caring for a cohort of Medicare beneficiaries. The financial risks and potential rewards are generally greater in the Next Generation program than in the Shared Savings program.
The big unknown for ACOs in both programs is whether the pandemic will dramatically increase costs, because of the need to care for an influx of beneficiaries suffering from COVID-19, or reduce costs, because fewer beneficiaries will receive routine preventive care or scheduled/elective procedures. The consensus among the ACO executives in the survey is that it will be the former.
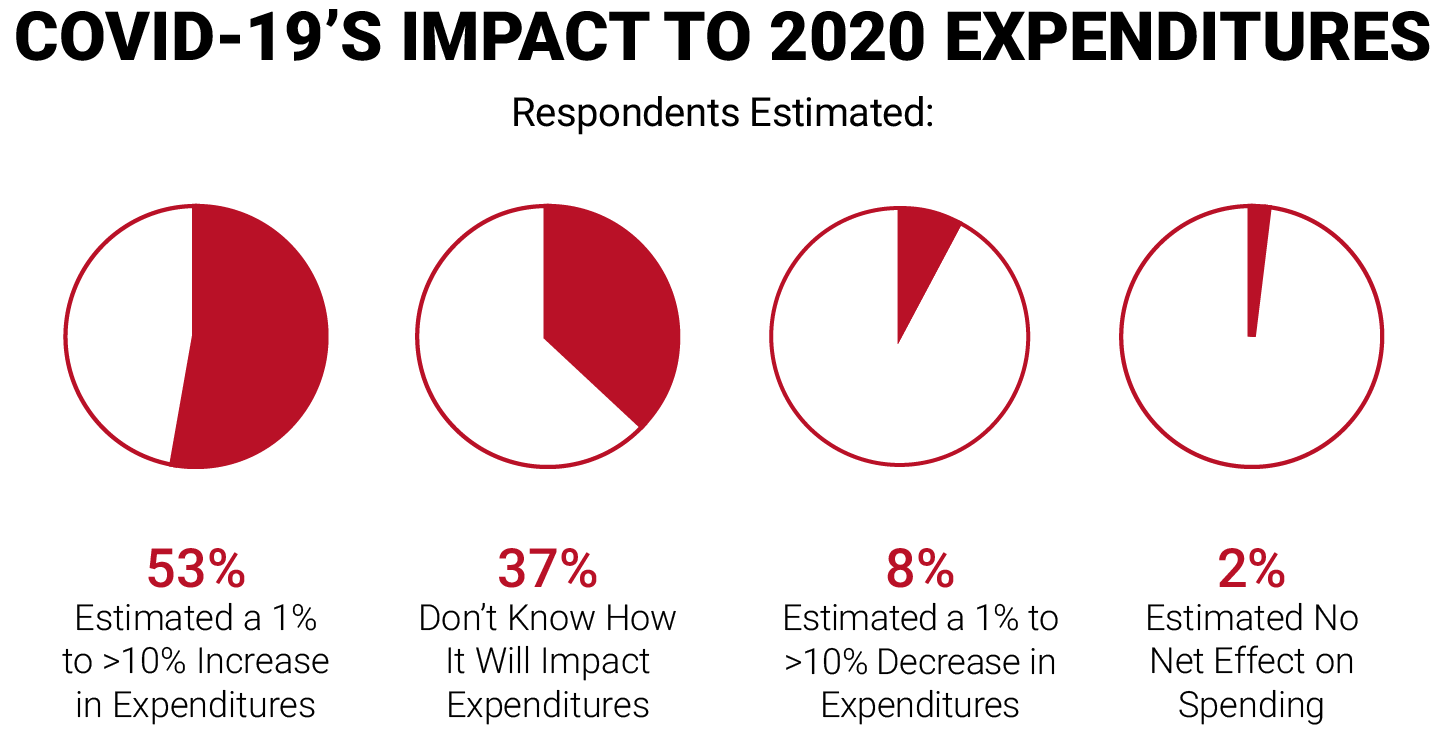
In summary, 97 percent of the ACO executives said there will be some degree of difficulty in predicting the ACOs’ financial performance this year.
In response to these concerns, on April 28, 2020, the Centers for Medicare & Medicaid Services (CMS) issued an interim final rule to afford Medicare ACOs some protection and predictability in the face of the COVID-19 pandemic.
CMS won’t count COVID-19-related treatment revenue and expenses in the methodologies that it uses to evaluate the performance of Medicare ACOs
In the rule, CMS invoked the “extreme and uncontrollable circumstances” provision in its ACO program, in order to offer relief related to the COVID-19 public health emergency (PHE). That provision protects ACOs from unforeseen occurrences like natural disasters that can cause their revenues or expenses to fluctuate in one direction or the other.
As a result, CMS won’t count COVID-19-related treatment revenue and expenses in the methodologies that it uses to evaluate the performance of Medicare ACOs. CMS will apply this protection retroactively to January 2020, and it will remain in effect until CMS determines that the COVID-19 PHE is over.
CMS also said participating ACOs can renew their risks contracts automatically for 2021 without re-applying, and that they can maintain their risks for 2021 at the same levels as they have for 2020.
“The rule is a fair way to handle ACO performance during a global public health pandemic,” NAACOS said in a statement reacting to the interim final rule. “We’re appreciative of the thoughtful ways CMS will modify the Shared Savings Program during the public health emergency, especially by removing spending associated with COVID-19 patients from performance calculations.”
TAKEAWAY
Certainly, a global pandemic is a once-in-a-lifetime event, and call for equally rare measures from the federal government to mitigate its financial impacts. Still, what’s happening should drive home the point that your hospital, health system or medical practice needs complete visibility into the health of your patient population if you’re going to succeed at value-based care.
You should have or develop the capability to:
- Stratify your patient population based on the severity of patients’ risk factors
- Create disease registries and manage patient cohorts
- Understand the health conditions in your patient population to develop proactive informational outreach campaigns
- Improve patient engagement and clinical outcomes
- Identify opportunities to provide and enhance prevention and wellness services
If your hospital, health system or medical practice participates in a Medicare ACO in either the Shared Savings Program or the Next General ACO program, you should work to understand how the coronavirus outbreak will affect both your revenue and cost projections, and how CMS’ latest actions will affect your operations.